Budding surgeons may soon train on stretchy, lifelike 3D-printed skin that oozes out blood and pus when cut.
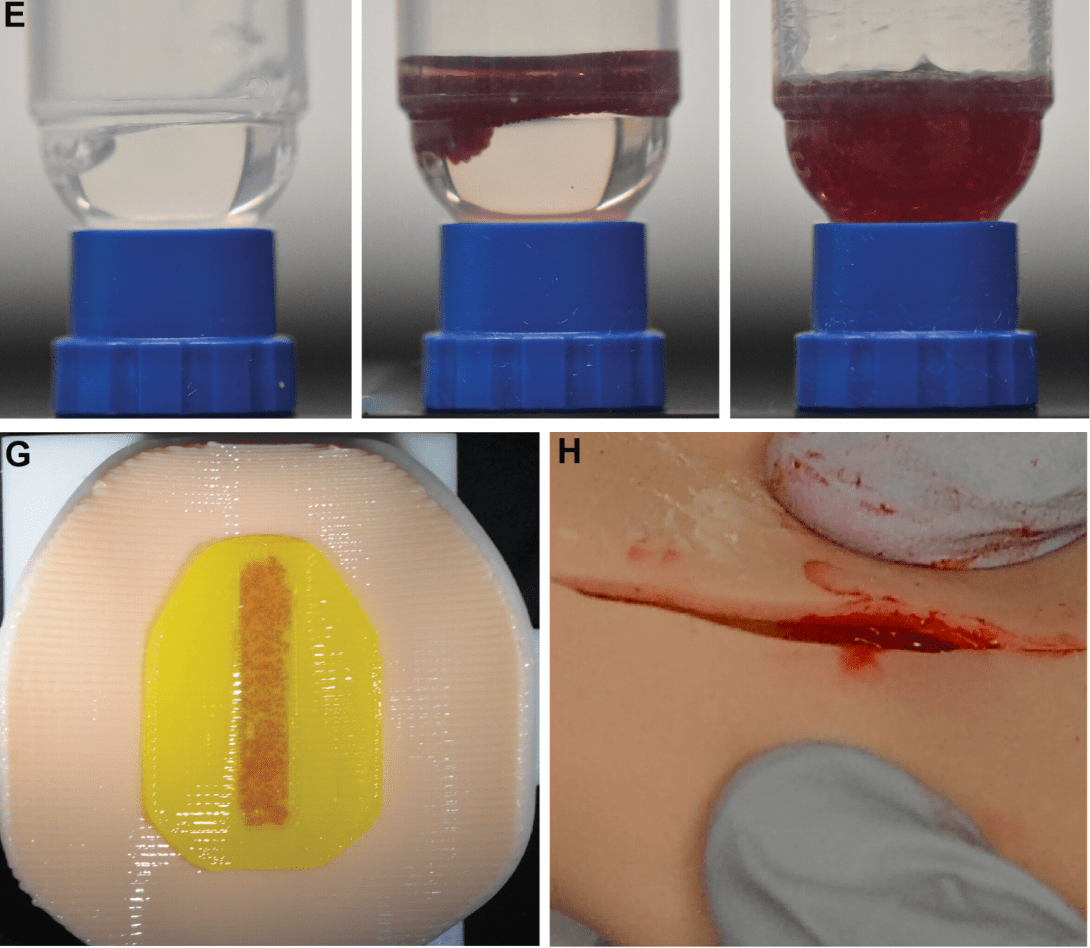
A new printable material developed by researchers at the University of Minnesota Twin Cities more closely mimics the adaptive nature of human tissue. It utilizes advances in modern bioprinting to produce lifelike tissue that’s stiffness can change depending on its location on a body and in what direction it is intended to move. For added realism, the researchers incorporated fluid-filled microcapsules into the printed material to simulate the release of bodily fluids.
Researchers believe their new 3D-printed tissue could be adapted and customized in the future to help create a variety of synthetic organs. Those on-demand, realistic substitutes could potentially expedite training for healthcare professions. The advancement, detailed this week in Science Advances, is just the latest in a string of studies highlighting how creepily lifelike synthetic skins have become.
“This approach opens the door to creating more realistic training models for surgery, which could ultimately improve medical outcomes,” University of Minnesota Department of Mechanical Engineering Ph.D graduate and paper first author Adarsh Somayaji said in a statement.
Making fake skin feel real
Fake skin in medical settings dates back centuries. Today’s versions are typically made by casting various synthetic materials into bodily shapes. These casts are invaluable tools for teaching surgeons, but they fall short of being a true one-to-one proxy for cutting into real human skin. The University of Minnesota researchers thought modern 3D bioprinters could change that, offering a way to create more structurally accurate and patient-specific organ models.
To do that, the researchers first developed a mathematical model to predict how their printed tissue should behave in the real world. This model helped ensure the skin would accurately replicate variations in stretchiness, stiffness, and strength, depending on where it is found on the body.

A time-lapse video released by the researchers shows the bioprinter laying down layers of synthetic skin with liquid-filled capsules embedded between them. One of the researchers then took the skin (which was fitted around a mannequin’s arm) and sliced into it with a razor blade. The fake blood trapped between the layers bursts out at the incision point, replicating in gruesome detail the sensation of real bleeding.
So far, it seems like the printed skin is performing as intended. In surveys conducted after practice sessions, surgeons reported that they preferred its tactile feedback and cutting response over the conventional fake skin they typically use.
”We anticipate that these tools can help bridge the gap in realism and mechanical fidelity between tissue simulants and real human tissue, thereby improving the quality of medical training and education as well as surgical outcomes,” the researchers write.
We’re quickly approaching an era of printable body parts
Simulated, synthetic skin has advanced rapidly from a sci-fi concept to real-world application in recent years. Earlier this summer, researchers from the University of Cambridge and University College London developed a new type of responsive synthetic skin made from a single hydrogel that can detect touch, pressure, heat, cold, and even damage. Eventually, researchers say that reactive skin could help humanoid robots “feel” the world around them.
Researchers from Graz University of Technology and the Vellore Institute of Technology (VIT) in India are similarly developing an artificial animal skin made of 3D-printed hydrogel layers and reinforced with living human cells. Though still in the research phase, that team believes it could mimic human skin accurately enough to replace the current need for animal skin in cosmetic testing.
These advancements are happening alongside improvements in the underlying hardware used to create them. Modern bioprinters, such as one developed by researchers at the University of Melbourne, can produce multiple types of structures that mimic a wide range of tissues, from soft skin to firmer cartilage and bone.
The end goal of all of this is to both improve the types of material future professionals train on and also, one day, potentially produce ready-made organs that could be used to provide transplants for patients who need them.
“While challenges remain in scaling up the process, we see strong potential for this 3D printing method in low-volume, high-complexity training scenarios,” Somayaji added.